The Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) Model is announcing a coordinated set of changes starting in performance year 2025 (PY 2025) in response to findings from the PY 2022 Global and Professional Direct Contracting Model Evaluation Report and feedback from interested parties. The changes include adjusting the financial methodology to reduce net losses to CMS as described in the PY 2022 Evaluation Report, improving the accuracy of benchmarks in response to feedback, and strengthening operational flexibility and risk management. For more information please visit the ACO REACH Model Performance Year 2025 Model Update Quick Reference.
The ACO Realizing Equity, Access, and Community Health (ACO REACH) Model provides novel tools and resources for health care providers to work together in an accountable care organization (ACO) to improve the quality of care for people with Traditional Medicare. REACH ACOs are comprised of different types of providers, including primary and specialty care physicians. To help advance health equity, the ACO REACH Model requires all participating ACOs to have a robust plan describing how they will meet the needs of people with Traditional Medicare in underserved communities and make measurable changes to address health disparities. Additionally, the model uses an innovative payment approach to better support care delivery and coordination for people in underserved communities.
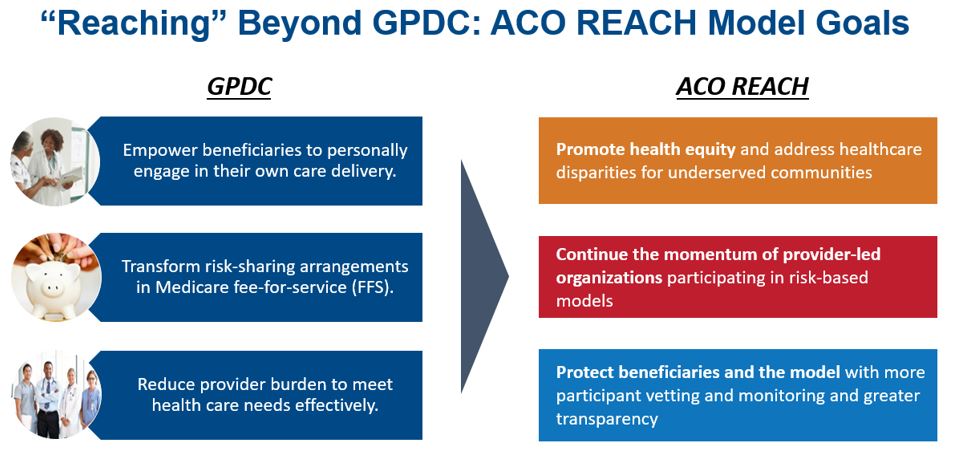
The ACO REACH Model makes important changes to the previous Global and Professional Direct Contracting (GPDC) Model in three areas:
This interactive map allows you to select any area to view more detailed information. Use the legend to understand the map symbols and colors.
Select anywhere on the map below to view the interactive version Source: Centers for Medicare & Medicaid Services Participants:Dark Blue: ACO REACH, ]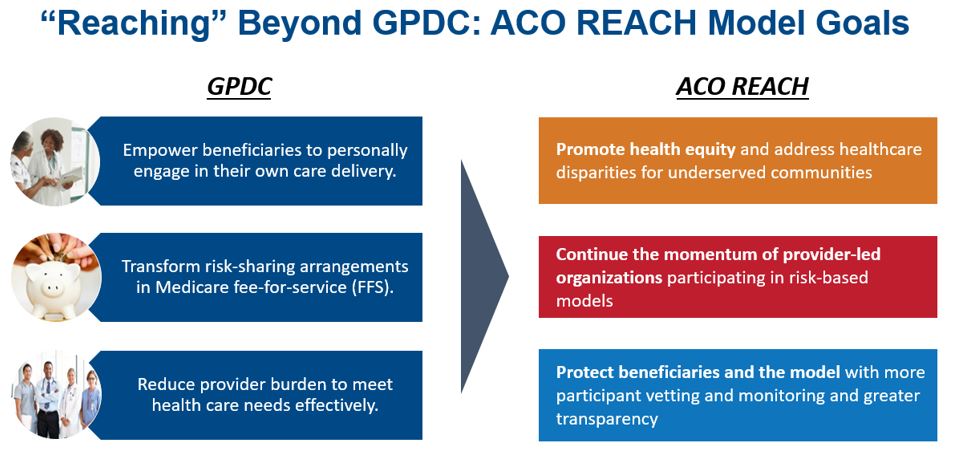
Please see the ACO REACH GPDC Comparison Table (PDF) for a comprehensive set of policy updates.
The first Performance Year of the redesigned model began on January 1, 2023 and will run for four Performance Years: Performance Year 2023 (PY2023) through PY2026. CMS has released a Request for Applications (RFA) for organizations interested in beginning participation in PY2023. Accepted applicants will have the option of participating in an Implementation Period leading up to PY2023, which runs from August 1, 2022 through December 31, 2022. Current GPDC Model participants must maintain a strong compliance record and agree to meet requirements for the redesigned model by January 1, 2023 in order to continue their participation.
The ACO REACH Model is focused on provider-based organizations and offers three types of participants:
There are two voluntary risk-sharing options under the ACO REACH Model. In each option, participating providers accept Medicare claims reductions and agree to receive at least some compensation from their ACO.
For future performance years under the ACO REACH Model, CMS intends that ACOs, Participant Providers, and Preferred Providers will receive the same scope of protection currently available for PY2021 and PY2022 of the GPDC Model under the CMS-sponsored model safe harbor at 42 CFR 1001.952(ii).
For reference, the following language appears on the GPDC Model webpage: CMS has determined that, beginning April 1, 2021, the anti-kickback statute safe harbor for CMS-sponsored model arrangements (42 CFR § 1001.952(ii)(1)) is available to protect certain DCE financial arrangements between or among the DCE, one or more DC Participant Providers, one or more Preferred Providers, or a combination thereof, provided that such arrangements comply with the requirements set forth in Section 3.04.M.1 of the GPDC Model Performance Period Participation Agreement (“Participation Agreement”). (Unless otherwise specified, capitalized terms have the meaning set forth in the Participation Agreement. Further, CMS has determined that, beginning April 1, 2021, the anti-kickback statute safe harbor for CMS-sponsored model patient incentives (42 CFR § 1001.952(ii)(2)) is available to protect certain in-kind patient incentives and Beneficiary Engagement Incentives furnished by a DCE, DC Participant Provider, or Preferred Provider to a Beneficiary or DC Beneficiary (as applicable), provided that such incentives are furnished in a manner that complies with the requirements set forth in Section 5.08.B of the Participation Agreement.
Please refer to the ACO REACH Model RFA (PDF) for additional details.
The application period for Performance Year 2023 closed and information on the selection process, including lists of organizations that have been accepted to participate in the Model starting January 1, 2023 and the subset participating in the optional Implementation Period (August 1, 2022 through December 31, 2022), is included on this webpage.
If you are interested in receiving CMS Innovation Center updates, including about the ACO REACH Model, subscribe to the CMS Innovation Center listserv.
If you are interested in receiving additional information and updates specifically about the ACO REACH Model, please subscribe to the ACO REACH Model listserv.
For any questions, please email the ACO REACH Model team at ACOREACH@cms.hhs.gov.
CMS recognizes that stakeholders are interested in information about models, including greater insights into the participants, what they are doing to improve care, and impacts on quality and costs in advance of evaluation results being published. CMS is committed to providing greater transparency into the ACO REACH Model.
For the ACO REACH Model, CMS will share the following information, regarding each REACH ACO participating in the model:
CMS will also share aggregate information for all REACH ACOs on quality and financial performance based on operations data and financial benchmarks, not evaluation, which will be updated quarterly. It is important to note that the quality information presented will be for two claims-based measures—All Cause Readmissions and Unplanned Admissions for Multiple Chronic Conditions. In addition, information will be shared on the payments being made to REACH ACOs on a quarterly basis.
A series of methodology papers will be published for the ACO REACH Model in the summer of 2024. These papers will be updates to the GPDC Model methodology papers, including all financial papers, which are available on the GPDC Model webpage .
Sign up for the ACO REACH listserv and continue to check this site for additional updates.